Countries facing severe shortages and poor distribution of health workers could benefit from training and deploying more mid-level health workers, such as midwives, nurses, medical assistants and surgical clinicians, according to a study published in the Bulletin of the World Health Organization today.
In countries where such health workers have been deployed, the clinical outcomes for certain services were just as good and – in some cases – even better than when physicians performed them, the study shows.
“Our findings de-bunk the myth that more extensive use of mid-level health workers might lead to services of poorer quality; despite the limitations of the evidence, it seems that in some areas they actually out-performed physicians,” said lead author Dr Zohra S. Lassi, Senior Instructor in the Division of Women and Child Health at the Aga Khan University in Karachi, Pakistan. “Most of our findings point to opportunities that all countries – rich and poor alike – can exploit.”
The study shows that when care for mothers and newborn babies is provided by midwives, as opposed to physicians working with midwives, the rates are lower for episiotomy (a surgical incision to ease a baby’s delivery that can lead to complications) and the use of painkillers. In addition, patient satisfaction is often higher, the study shows.
Another important finding is that care provided by nurses in various fields of health – including prevention and treatment of heart disease, diabetes, mental health conditions and HIV infection – is as effective as that provided by physicians. There is no suggestion in the study that physicians should be entirely replaced by mid-level health workers but that in certain health areas mid-level health workers do just as well, if not better than physicians.
The study is one of a collection of articles in a special issue of the international public health journal devoted to the topic of: the health workforce needed in countries to move towards or sustain universal coverage of health services. The new study analyses 53 studies conducted in 18 countries over the last 20 years comparing the outcomes of certain types of care provided by mid-level health workers and of the care provided by physicians. It is the first systematic review – a study that analyses all the available evidence – to make such a comparison.
Most of the studies analysed compare either: the care provided by midwives with that provided by doctors working in a team with midwives; or, the care provided by nurses with that provided by doctors.
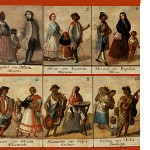
More than half of the 53 studies were done at tertiary care facilities in high-income countries (Australia, Canada, Italy, the Netherlands, Sweden, the United Kingdom and the United States of America). The rest were in middle-income (Cameroon, China, the Philippines, South Africa, Thailand, Turkey and Viet Nam) and low-income countries (Malawi, Mozambique, Nepal and the United Republic of Tanzania), according to the World Bank income level categories. The study’s results are particularly relevant for countries striving to provide their people with universal access to affordable, quality health-care services – an endeavour for which a suitable health workforce is a key component. In 2012, the United Nations General Assembly adopted a resolution urging governments to commit themselves to universal health coverage.
“Moving towards or sustaining universal health coverage is a challenge for all countries: traditional models of care, dominated by physician-led provision of expensive curative services in tertiary care facilities, have their limitations,” said Dr Giorgio Cometto, adviser to the executive director of the Global Health Workforce Alliance, a WHO partnership.
“But when mid-level health workers are given a more prominent role, health-care services may respond better to citizens’ needs – and this approach may also save money in the long-run,” said Cometto, who is also one of the authors of the study. WHO encourages all countries to adopt the most efficient mix of health-care skills and cadres possible to address the health needs of their populations. It has issued recommendations on the delegation of tasks from one type of health worker to another in the care of HIV infection, and maternal and newborn health and offers technical support to countries facing health workforce challenges.
This special issue of the Bulletin of the World Health Organization provides examples of success stories in tackling health workforce challenges, and presents innovative approaches and new evidence for countries. Other articles in this issue can be provided under embargo on request. They include:
- Editorial: leadership action needed for health workforce development towards universal health coverage. Hon. Alexandre Padilha (Minister of Health, Brazil), Hon. Joseph Kasonde (Minister of Health, Zambia), Prof Ghufron Mukti (Indonesia), Hon. Keizo Takemi (Japan), Lord Nigel Crisp (UK), Prof Eric Buch (University of Pretoria, South Africa).
- Editorial: Investing in human resources for health: the need for a paradigm shift for the global health community over the next decade. Feng Zhao (African Development Bank), Neil Squires (DFID), David Weakliam (Irish Aid), Wim Van Lerberghe (University of Lisbon), Agnes Soucat (African Development Bank), Kadidiatou Toure (Partnership for Maternal and Child Health), George Shakarishvili (Global Fund to Fight AIDS, Tuberculosis and Malaria), Estelle Ouain (USAID), Akiko Maeda (World Bank).
- News feature: More midwives are needed globally to improve maternal and newborn health.
- Interview with Dr Francisco Eduardo de Campos about Brazil’s efforts to distribute doctors more evenly in rural and poor urban areas.
- Policy and practice: Developing synergy among partners’ support towards countries in policy, and practice with enhanced investments for scaling up community health worker programmes. Kate Tulenko (Intrahealth)
- Policy and practice: Human resources for health, universal health coverage and the post-2015 development agenda: fostering equity and effective coverage. James Campbell (ICS Integrare)
- Perspectives: Leveraging information technology to address the health workforce gap. Bob Bollinger (Johns Hopkins Bloomberg School of Public Health, USA)
- Lessons from the field: Health workforce contributions to health system development: a platform for universal health coverage implementation. Viroj Tangcharoensathien (Thailand)
This news release is available in Spanish, French and Portuguese.